Stroke
Highlights
Signs of Stroke
The American Stroke Association advises everyone to learn to recognize these signs of stroke:
- Sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- Sudden confusion, trouble speaking or understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden, severe headache with no known cause
F.A.S.T.
The acronym FAST is an easy way to remember signs of stroke and what to do if you think a stroke has occurred. (The most important is to immediately call 9-1-1 for emergency assistance.) FAST stands for:
- (F)ACE. Ask the person to smile. Check to see if one side of the face droops.
- (A)RMS. Ask the person to raise both arms. See if one arm drifts downward.
- (S)PEECH. Ask the person to repeat a simple sentence. Check to see if words are slurred and if the sentence is repeated correctly.
- (T)IME. If a person shows any of these symptoms, time is essential. It is important to get to the hospital as quickly as possible. Call 9-1-1. Act FAST.
Clot-Busting Treatment Window Expanded
It is critical for patients with stroke symptoms to get to a hospital as quickly as possible. Patients who are suffering an ischemic stroke may be able to receive a clot-busting drug to dissolve the clot if they reach a hospital within 3 hours of symptom onset.
According to the American Heart Association and the American Stroke Association, this treatment window can be extended to 4.5 hours for patients who:
- Are younger than 80 years old
- Are not having a severe stroke
- Do not have a history of stroke and diabetes
- Do not take oral anticoagulant (“blood-thinner”) drugs
Drug Approval
In 2011, the Food and Drug Administration (FDA) approved a new anticoagulant drug, rivaroxaban (Xarelto), to prevent stroke and blood clots in patients with atrial fibrillation, a common irregular heart rhythm that is a major cause of stroke. Last year, the FDA approved dabigatran (Pradaxa) for the same purpose. These new anticoagulants may be an alternative to warfarin (Coumadin, generic) for some patients. The FDA is expected to announce in 2012 whether a third new anticoagulant, apixaban (Eliquis), will be approved.
Introduction
A stroke is the sudden death of brain cells due to lack of oxygen. A stroke is usually defined as one of two types:
- Ischemic (caused by a blockage in an artery)
- Hemorrhagic (caused by a tear in the artery's wall that produces bleeding into or around the brain)
The consequences of a stroke, the type of functions affected, and the severity depend on where in the brain it has occurred and the extent of the damage.
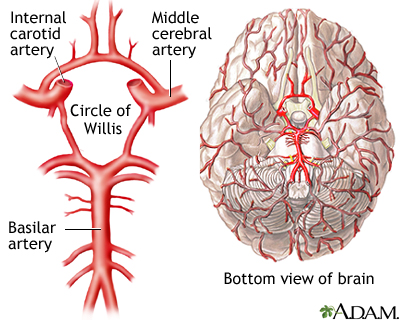
Blood Flow Blockage. Strokes are caused by either blood flow blockage to the brain (ischemic stroke) or the sudden rupture of an artery in the brain (hemorrhagic stroke). Brain cells require a constant supply of oxygen to stay healthy and function properly. Therefore, blood needs to be supplied continuously to the brain through two main arterial systems:
- The carotid arteries come up through either side of the front of the neck. (To feel the pulse of a carotid artery, place your fingertips gently against either side of your neck, right under the jaw.)
- The basilar artery forms at the base of the skull from the vertebral arteries, which run up along the spine, join, and come up through the rear of the neck.
Blockage of blood flow to the brain for even a short period of time can be disastrous and cause brain damage or even death.
Ischemic Stroke
Ischemic strokes are by far the more common type, causing nearly 90% of all strokes. Ischemia means the deficiency of oxygen in vital tissues. Ischemic strokes are caused by blood clots that are usually one of four types.
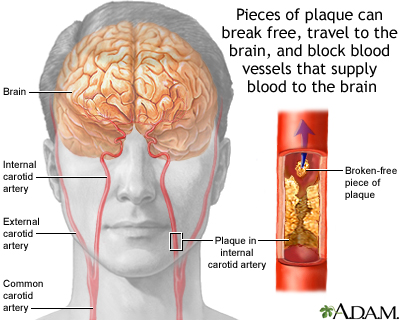
Thromboembolic Stroke and Atherosclerosis. These types of stroke usually occur when an artery that carries blood to the brain is blocked by a thrombus (blood clot) that forms as the result of atherosclerosis (commonly known as hardening of the arteries). These strokes are also sometimes referred to as large-artery strokes. The process leading to thrombotic stroke is complex and occurs over time:
- The arterial walls slowly thicken, harden, and narrow until blood flow is reduced, a condition known as stenosis.
- As these processes continue, blood flow slows.
In addition, other events contribute to the coming stroke:
- The artery is narrowed by a cholesterol-laden plaque that becomes susceptible to tearing. In this event, the thrombus (blood clot) forms.
- The blood clot then breaks off and travels to the brain, where it blocks an artery and shuts off oxygen to part of the brain. A stroke occurs.
Cardioembolic Strokes and Atrial Fibrillation. An embolic stroke is caused by a dislodged blood clot that has traveled through the blood vessels (an embolus) until it becomes wedged in an artery. Cardioembolic strokes start with clots in the heart and may be due to various conditions:
- In many cases, the blood clots originally form as a result of a heart rhythm disorder known as atrial fibrillation.
- Emboli can also originate from blood clots that form at the site of artificial heart valves.
- Patients with heart valve disorders such as mitral stenosis are at increased risk for clots when they also have atrial fibrillation.
- Emboli can also occur after a heart attack or in association with heart failure.
- Rarely, emboli are formed from fat particles, tumor cells, or air bubbles that travel through the bloodstream.
Thrombotic Strokes. Thrombotic strokes occur when a clot develops in a diseased artery right in the brain. Thrombotic strokes are less common than either type of embolic strokes. Thrombotic strokes tend to occur at night, and their symptoms may develop in a stuttering fashion, more slowly than those of an embolic stroke, which is usually swift and sudden.
Small Vessel (Lacunar) Strokes. Lacunar infarcts are a series of very tiny, ischemic strokes, which cause clumsiness, weakness, and emotional variability. They make up the majority of silent brain infarctions and are probably a result of chronic high blood pressure. They are actually a subtype of thrombotic stroke. They can also sometimes serve as warning signs for a major stroke.
Many elderly people have had silent brain infarctions, small strokes that cause no apparent symptoms. They are detected in up to half of elderly patients who undergo imaging tests for problems other than stroke. The presence of silent infarctions indicates an increased risk for future stroke, as well as dementia. Smokers and people with hypertension are at particular risk.
Transient Ischemic Attacks (TIAs)
A transient ischemic attack (TIA) is an episode in which a person has stroke-like symptoms that typically last for a few minutes and usually less than 1 - 2 hours. Transient ischemic attacks (TIAs) are caused by tiny emboli (clots often formed of pieces of calcium and fatty plaque) that lodge in an artery to the brain. They typically break up quickly and dissolve, but they do temporarily block the supply of blood to the brain.
TIAs do not cause lasting damage, but they are a warning sign that a true stroke may happen in the future if something is not done to prevent it. TIA should be taken very seriously and treated as aggressively as a stroke. About 10 - 15% of patients who have a TIA have a stroke within 3 months, with half of these strokes occurring within 48 hours after the TIA.
Hemorrhagic Stroke
About 10% of strokes occur from hemorrhage (sudden bleeding) into or around the brain. While hemorrhagic strokes are less common than ischemic strokes, they tend to be more deadly.
Hemorrhagic strokes are categorized by how and where they occur.
- Parenchymal, or intracerebral, hemorrhagic strokes. These strokes occur from bleeding within the brain tissue. They are most often the result of high blood pressure exerting excessive pressure on arterial walls already damaged by atherosclerosis. Heart attack patients who have been given drugs to break up blood clots or blood-thinning drugs have a slightly increased risk for this type of stroke.
- Subarachnoid hemorrhagic strokes. This kind of stroke occurs when a blood vessel on the surface of the brain bursts, leaking blood into the subarachnoid space, an area between the brain and the skull. They are usually caused by the rupture of an aneurysm, a bulge in a blood vessel, which creates a weakening in the artery wall.
- Arteriovenous malformation (AVM) is an abnormal connection between arteries and veins. If it occurs in the brain and ruptures, it can also cause a hemorrhagic stroke.
Risk Factors
New or recurrent strokes affect about 795,000 Americans every year. On average, someone in the United States has a stroke every 40 seconds. While age is the major risk factor, people who have a stroke are likely to have more than one risk factor.
Age
People most at risk for stroke are older adults, particularly those who have high blood pressure, are sedentary, are overweight, smoke, or have diabetes. Older age is also linked with higher rates of post-stroke dementia. Younger people are not immune, however. Many stroke victims are under age 65.
Gender
In most age groups, except older adults, stroke is more common in men than in women. However, stroke kills more women than men. This may be partly due to the fact that women tend to live longer than men, and stroke is more common among older adults. Women account for about 6 in 10 stroke deaths. For younger women, birth control pills and pregnancy can increase the risk of stroke.
Race and Ethnicity
All minority groups, including Native Americans, Hispanics, and African-Americans, face a significantly higher risk for stroke and death from stroke than Caucasians. African-Americans have twice the risk for first-time stroke as Caucasians. The differences in risk among all groups diminish as people age.
The greatest disparity in risk occurs in young adults. Younger African-Americans are two to three times more likely to have a stroke than their Caucasian peers and four times more likely to die from one. They also face a higher risk for death from heart disease. African-Americans have a higher prevalence of obesity, diabetes, and hypertension than other groups. However, studies suggest that socioeconomic factors also affect these differences.
Family History
A family history of stroke or TIA is a strong risk factor for stroke.
Lifestyle Factors
Smoking. People who smoke a pack a day have more than twice the risk for stroke as nonsmokers. Smoking increases both hemorrhagic and ischemic stroke risk. The risk for stroke may remain elevated for as long as 14 years after quitting, so the earlier one quits the better.
Diet. Unhealthy diet (saturated fat, high sodium) can contribute to heart disease, high blood pressure, and obesity, which are all risk factors for stroke.
Physical Inactivity. Lack of regular exercise can increase the risk of obesity, diabetes, and poor circulation, which increase the risk of stroke.
Alcohol and Drug Abuse. Alcohol abuse, including binge drinking, increases the risk of stroke. Drug abuse, particularly with cocaine or methamphetamine, is a major factor of stroke in young adults. Anabolic steroids, used for body-building and sports enhancement, also increase stroke risk.
Heart and Vascular Diseases
Heart disease and stroke are closely tied for many reasons. People who have one heart or vascular condition (such as high blood pressure, high cholesterol, heart disease, diabetes, or peripheral artery disease) are at increased risk for developing other related conditions.
Prior Stroke. A history of a prior stroke or TIA significantly increases the risk for a subsequent stroke. People who have had at least one TIA are 10 times more likely to have a stroke than those who have not had a TIA.
Prior Heart Attack. People who have had a heart attack are at increased risk of stroke.
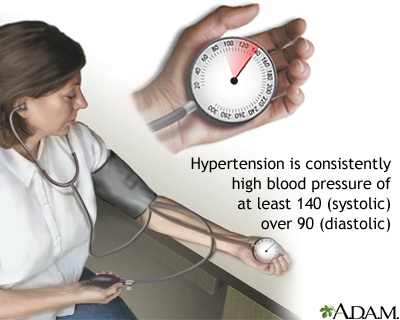
High Blood Pressure. High blood pressure (hypertension) contributes to about 70% of all strokes. People with hypertension have up to 10 times the normal risk of stroke, depending on the severity of the blood pressure and the presence of other risk factors. Hypertension is also an important cause of so-called silent cerebral infarcts (“mini-strokes” caused by blockages in the blood vessels in the brain), which may predict major stroke. Controlling blood pressure is extremely important for stroke prevention.
Unhealthy Cholesterol Levels. A high total cholesterol level increases the risk of developing atherosclerosis (“hardening of the arteries”) and heart disease. In atherosclerosis, fatty deposits (plaques) of cholesterol build up in the arteries of the heart.
Heart Disease. Coronary artery disease (heart disease), which is the end result of atherosclerosis, increases stroke risk. Anti-clotting medications, which are used in heart disease treatment to break up blood clots, can increase the risk of hemorrhagic stroke.
Atrial Fibrillation. Atrial fibrillation, a major risk factor for stroke, is a heart rhythm disorder in which the atria (the upper chambers in the heart) beat very rapidly and irregularly. The blood stagnates instead of being pumped out promptly, increasing the risk for formation of blood clots that break loose and travel toward the brain. Between 2 - 4% of patients with atrial fibrillation without any history of TIA or stroke will have an ischemic stroke over the course of a year. The risk is generally highest for those older than age 75, with heart failure or enlarged heart, coronary artery disease, history of clots, diabetes, or heart valve abnormalities.
Structural Heart Problems. Dilated cardiomyopathy (enlarged heart), heart valve disorders, and congenital heart defects, such as patent foramen ovalae (opening in chambers of heart) and atrial septal aneurysm (bulging of heart chamber), are risk factors for stroke.
Carotid Artery Disease and Peripheral Artery Disease. Carotid artery disease is a serious risk factor for stroke. Atherosclerosis can cause fatty build-up in the carotid arteries of the neck, which can lead to blood clots that block blood flow and oxygen to the brain. People with peripheral artery disease, which occurs when atherosclerosis narrows blood vessels in the legs and arms, are at increased risk of carotid artery disease and subsequently stroke.
Diabetes
Heart disease and stroke are the leading causes of death in people with diabetes. Diabetes is second only to high blood pressure as the main risk factor for stroke. The risk is highest for adults newly diagnosed with type 2 diabetes and patients with diabetes who are younger than age 55. African-Americans with diabetes are at even higher risk for stroke at a younger age. Diabetes is a particularly strong risk factor for ischemic stroke, perhaps because of accompanying risk factors such as obesity and high blood pressure. Diabetes does not appear to increase the risk for hemorrhagic stroke.
Obesity and Metabolic Syndrome
Obesity may increase the risk for both ischemic and hemorrhagic stroke independently of other risk factors that often co-exist with excess weight, including diabetes, high blood pressure, and unhealthy cholesterol level. Weight that is centered around the abdomen (the so-called apple shape) has a particularly high association with stroke, as it does for heart disease, in comparison to weight distributed around hips (pear-shape).
Obesity is particularly hazardous when it is one of the components of metabolic syndrome. This syndrome is diagnosed when three of the following conditions are present: abdominal obesity, low HDL cholesterol, high triglyceride levels, high blood pressure, and insulin resistance. Because metabolic syndrome is a pre-diabetic condition that is significantly associated with heart disease, people with this syndrome are at increased risk for stroke even before diabetes develops.
Other Risk Factors
Migraine. Studies suggest that migraine or severe headache may be a risk factor for stroke in both men and women, especially before age 50. Overall, 2 - 3% of ischemic strokes occur in people with a history of migraine. However, in patients under age 45, about 15% of all strokes (and 30 - 60% of strokes in young women) are associated with a history of migraines, particularly migraine with aura. For young women with migraines, other risk factors (such as high blood pressure, smoking, and use of estrogen-containing oral contraceptives) may increase stroke risk.
Sickle Cell Disease. People with sickle cell disease are at increased risk for stroke at a young age.
Pregnancy. Pregnancy carries a very small risk for stroke, mostly in women with pregnancy-related high blood pressure. The risk appears to be higher in the postpartum (post-delivery) period, perhaps because of the sudden change in circulation and hormone levels.
Depression. Some research suggests that depression may increase the risk for stroke.
NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin, generic) and diclofenac (Cataflam, Voltaren, generic) may increase the risk of stroke, especially for patients who have other stroke risk factors.
Prognosis
Stroke is the fourth leading cause of death in the United States. Mortality rates are declining, however. Over 75% of patients survive a first stroke during the first year, and over half survive beyond 5 years.
Severity of an Ischemic Versus Hemorrhagic Stroke
People who suffer ischemic strokes have a much better chance for survival than those who have hemorrhagic strokes. Among the ischemic stroke categories, the greatest dangers are posed by embolic strokes, followed by thrombotic and lacunar strokes.
Hemorrhagic stroke not only destroys brain cells but also poses other complications, including increased pressure on the brain or spasms in the blood vessels, both of which can be very dangerous. Studies suggest, however, that survivors of hemorrhagic stroke have a greater chance for recovering function than those who survive ischemic stroke.
Long-Term Complications and Disabilities
Many patients are left with physical weakness and often have accompanying pain and spasticity (muscle stiffness or spasms). Depending on the severity of the symptoms and how much of the body is involved, these impairments can affect the ability to walk, to rise from a chair, to feed oneself, to write or use a computer, to drive, and many other activities.
Factors that Affect Quality of Life in Survivors
Many stroke survivors recover functional independence after a stroke, but 25% are left with a minor disability and 40% experience moderate-to-severe disabilities. The National Institutes of Health (NIH)'s stroke scale helps predict the severity and outcome of a stroke by scoring 11 factors (levels of consciousness, gaze, visual fields, facial movement, motor functions in the arm and leg, coordination, sensory loss, problems with language, inability to articulate, and attention).
Patients with ischemic strokes who score less than 10 have a favorable outlook after a year, while only 4 - 16% of patients do well if their score is more than 20.
Factors Affecting Recurrence
The risk for recurring stroke is highest within the first few weeks and months of the previous stroke. But about 25% of people who have a first stroke will go on to have another stroke within 5 years. Risk factors for recurrence include:
- Older age
- Evidence of blocked arteries (a history of coronary artery disease, carotid artery disease, peripheral artery disease, ischemic stroke, or TIA)
- Hemorrhagic or embolic stroke
- Diabetes
- Alcoholism
- Valvular heart disease
- Atrial fibrillation
Symptoms
People at risk and partners or caretakers of people at risk for stroke should be aware of its typical symptoms. The stroke victim should get to the hospital as soon as possible after these warning signs appear. It is particularly important for people with migraines or frequent severe headaches to understand how to distinguish between their usual headaches and symptoms of stroke.
Time is of the essence in treating stroke. Studies show that patients receive faster treatment for stroke if they arrive by ambulance rather than coming to the emergency room on their own. People should immediately call 911 for emergency assistance if they have any of warning signs of stroke:
- Sudden numbness or weakness of the face, arm or leg, especially on one side of the body
- Sudden confusion, trouble speaking or understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden, severe headache with no known cause
An easy way to remember the signs of stroke, and what to do, is by the acronym "F.A.S.T." If you think you or someone else is having a stroke, the National Stroke Association's F.A.S.T. test advises:
- (F)ACE. Ask the person to smile. Check to see if one side of the face droops.
- (A)RMS. Ask the person to raise both arms. See if one arm drifts downward.
- (S)PEECH. Ask the person to repeat a simple sentence. Check to see if words are slurred and if the sentence is repeated correctly.
- (T)IME. If a person shows any of these symptoms, time is essential. It is important to get to the hospital as quickly as possible. Call 9-1-1. Act FAST.
Symptoms of TIAs and Early Ischemic Stroke
The symptoms of a transient ischemic attack (TIA) and early ischemic stroke are similar. In the case of a TIA, however, the symptoms resolve within 24 hours. Symptoms depend on where the injury in the brain occurs. The origin of the stroke is usually either the carotid or basilar arteries.
Symptoms From Blockage in the Carotid Arteries. The carotid arteries stem off of the aorta (the primary artery leading from the heart) and lead up through the neck, around the windpipe, and into the brain. When TIAs or strokes result from clots that form on blockages in the carotid artery, symptoms may occur in either the retina of the eye or the cerebral hemisphere (the large top part of the brain).
Symptoms include:
- When oxygen to the eye is reduced, people describe the visual effect as a shade being pulled down. People may develop poor night vision. About 35% of TIAs are associated with temporary lost vision in one eye. The visual impairment occurs on the same side as the carotid disease.
- When the cerebral hemisphere is affected, a person can have problems with speech and partial and temporary paralysis, drooping eyelid, tingling, and numbness, usually on one side of the body. The stroke victim may be unable to express thoughts verbally or to understand spoken words. If the stroke injuries are on the right side of the brain, the symptoms will develop on the left side of the body and vice versa.
- Uncommonly, patients may have seizures.
Symptoms From Blockage in the Basilar Artery. The basilar artery is formed at the base of the skull from the vertebral arteries, which run up along the spine and join at the back of the head. When stroke or TIAs originate here, both hemispheres of the brain may be affected so that symptoms occur on both sides of the body. The following symptoms may develop:
- Temporarily dim, gray, blurry, or lost vision, usually in both eyes
- Tingling or numbness in the mouth, cheeks, or gums
- Headache, usually in the back of the head
- Dizziness
- Nausea and vomiting
- Difficulty swallowing
- Weakness in the arms and legs, sometimes causing a sudden fall
Such strokes usually occur in the brain stem, which can have profound effects on breathing, blood pressure, heart rate, and other vital functions, but have no affect on thinking or language.
Speed of Symptom Onset. The speed of symptom onset of a major ischemic stroke may indicate its source:
- If the stroke is caused by an embolus (a clot that has traveled to an artery in the brain), the onset is sudden. Headache and seizures can occur within seconds of the blockage.
- When thrombosis (a blood clot that has formed within the brain) causes the stroke, the onset usually occurs more gradually, over minutes to hours. On rare occasions it progresses over days to weeks.
Symptoms of Hemorrhagic Stroke
Intracerebral Hemorrhage Symptoms. Symptoms of an intracerebral, or parenchymal, hemorrhage typically begin very suddenly, evolve over several hours, and include:
- Severe headache
- Nausea and vomiting
- Altered mental states
- Seizures
Subarachnoid Hemorrhage. When the hemorrhage is a subarachnoid type, warning signs may occur from the leaky blood vessel a few days to a month before the aneurysm fully develops and ruptures. Warning signs may include:
- Sudden onset of severe headache
- Nausea and vomiting
- Sensitivity to light
- Various neurologic abnormalities. Seizures, for example, occur in about 8% of patients.
When the aneurysm ruptures, the stroke victim may experience:
- A terrible headache
- Neck stiffness
- Vomiting
- Altered states of consciousness
- Eyes may become fixed in one direction or lose vision
- Stupor, rigidity, and coma
Diagnosis
A diagnostic work-up for stroke includes physical and neurological examinations, patient’s medical history, blood tests (to measure blood glucose levels, blood coagulation time, cardiac enzymes, and other factors), and imaging tests. Many of the same procedures are used to diagnose a stroke and to evaluate the risk of future major stroke in patients who have had a transient ischemic attack (TIA).
For patients who have suffered a major stroke, the first step is to determine as quickly as possible whether the stroke is ischemic (caused by blood clot blockage) or hemorrhagic (caused by bleeding). Clot-busting drug therapies can be life-saving for ischemic stroke patients, but they are most effective only in the first 3 - 4 hours. However, if the stroke is caused by a hemorrhage, thrombolytic drugs will likely increase the bleeding and can be lethal.
Imaging Tests Used for Stroke and Risk Factors for Stroke
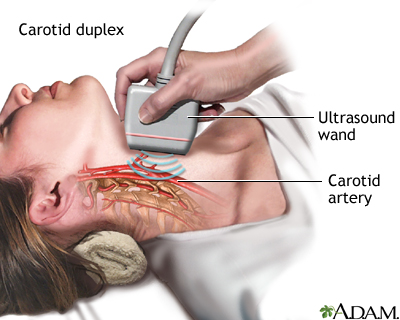
Carotid Ultrasound. Carotid ultrasound procedures such as carotid duplex are valuable tools for measuring the width of the artery and how the blood flows through it. Carotid ultrasound can help determine the severity of plaque build-up and narrowing and blocking of the carotid arteries (carotid stenosis).
Computed Tomography and Magnetic Resonance Imaging. Imaging tests can help distinguish between ischemic and hemorrhagic strokes. Computed tomography (CT) and magnetic resonance imaging (MRI) scans can help show signs of bleeding and can also help indicate whether a stroke is relatively new or recent.
MRIs are better than CT scans at differentiating between a hemorrhagic stroke and an ischemic stroke during the first few hours after symptoms begin. MRIs are also the preferred imaging technique for evaluating patients with probable TIA. However, an MRI can take longer to perform than a CT and is sometimes not as widely available. For these reasons, a CT scan may be used instead of MRI.
Cerebral Angiography. Cerebral angiography is an invasive procedure that may be used for patients with TIAs who need surgery. It can also detect aneurysms and monitor thrombolytic therapy. It requires the insertion of a catheter into the groin, which is then threaded up through the arteries to the base of the carotid artery. At this point a dye is injected, and x-rays, CTs, or MRI scans determine the location and extent of the narrowing, or stenosis, of the artery.
Magnetic Resonance Angiography (MRA) and Computerized Tomography Angiography. Magnetic resonance angiography and computerized tomography angiography are noninvasive ways of evaluating the carotid arteries and the arteries in the brain. In many situations, these tests can be used instead of cerebral angiography.
Heart Evaluation
Electrocardiogram (ECG). A heart evaluation using an electrocardiogram (ECG) is important in any patient with a stroke or suspected stroke. An ECG records the electrical current in the heart muscle.
Echocardiogram. An echocardiogram uses ultrasound to view the chambers and valves of the heart. It is generally useful for stroke patients to identify blood clots or risk factors for blood clots that can travel to the brain and cause stroke. There are two types of echocardiograms:
- Transthoracic echocardiograms (TTE) view the heart through the chest. It is noninvasive and is the standard approach.
- Transesophageal echocardiogram (TEE) examines the heart using an ultrasound tube that the patient swallows and passes down the throat. It is uncomfortable and requires sedation. It is typically used to obtain more accurate images of the heart if a TTE has suggested abnormalities, such as atrial fibrillation or patent foramen ovale (PFO).
ABCD2 Score
Patients who have a TIA are at increased risk for a major stroke in the days and weeks that follow. The ABCD2 score is a tool that helps doctors predict short-term stroke risk following a TIA. The ABCD2 score assigns points for various factors, including:
- Age (over 60 years)
- Blood pressure (greater or equal to 140/90 mm Hg)
- Clinical features (weakness on one side of the body, speech impairment without weakness)
- Duration of TIA symptoms (at least 60 minutes)
- Diabetes
Based on the number of points, a doctor can identify whether a patient is at low, moderate, or high risk of having a stroke within 2 days after a TIA. The ABCD2 score can help doctors better decide which patients need hospitalization and emergency care.
Treatment
Until recently, the treatment of stroke was restricted to basic life support at the time of the stroke and rehabilitation later. Now, however, treatments can be beneficial when administered as soon as possible after the onset of the stroke. It is critical to get to the hospital and be diagnosed as soon as possible. There are several steps in the initial assessment and management of a person with a stroke.
Receiving treatment early is essential in reducing the damage from a stroke. The chances for survival and recovery are also best if treatment is received at a hospital specifically certified as a primary stroke center.
Treatment of Ischemic Stroke
Immediate treatment of ischemic stroke aims at dissolving the blood clot. Patients who arrive at the emergency room with signs of acute ischemic stroke are usually given aspirin to help thin the blood. Aspirin can be lethal for patients suffering a hemorrhagic stroke, so it is best not to take aspirin at home and to wait until after the doctor has determined what kind of stroke has occurred.
If patients arrive at the hospital within 3 - 4 hours of stroke onset (when symptoms first appear), they may be candidates for thrombolytic (“clot-buster”) drug therapy. Thrombolytic drugs are used break up existing blood clots. The standard thrombolytic drugs are tissue plasminogen activators (t-PAs). They include alteplase (Activase) and reteplase (Retavase).
The following steps are critical before injecting a clot-buster drug:
- Before the thrombolytic is given, a CT scan must first confirm that the stroke is not hemorrhagic. If the stroke is ischemic, a CT scan can also suggest if injuries are very extensive, which might affect the use of thrombolytics.
- Thrombolytics must generally be administered within 3 - 4 hours of a stroke to have any effect. Best results are achieved if patients are treated with 90 minutes of a stroke.
- According to guidelines from the American Heart Association and American Stroke Association, some patients may benefit from treatment with a thrombolytic within 4.5 hours after stroke symptoms begin. These patients include those who are younger than 80 years, are having a less severe stroke, do not have a history of stroke or diabetes, and do not take anticoagulant (blood-thinner) drugs. Patients who do not meet these criteria should not be treated with a thrombolytic after the 3-hour window.
Thrombolytics carry a risk for hemorrhage, so they may not be appropriate for patients with existing risk factors for bleeding.
Treatment of Hemorrhagic Stroke
Treatment of hemorrhagic stroke depends in part on whether the stroke is caused by bleeding between the brain and the skull (subarachnoid hemorrhage) or within the brain tissue (intracerebral hemorrhage). Both medications and surgery may be used.
Medications. Various types of drugs are given depending on the cause of the bleeding. If high blood pressure is the cause, antihypertensive medications are administered to lower blood pressure. If anticoagulant medications, such as warfarin (Coumadin, generic) or heparin, are the cause, they are immediately discontinued and other drugs may be given to increase blood coagulation. Other drugs, such as the calcium channel blocker nimodipine (Nimotop), can help reduce the risk of ischemic stroke following hemorrhagic stroke.
Surgery. Surgery may be performed for aneurysms or arteriovenous malformations that are bleeding. The surgery may be done through a craniotomy, which involves making an opening in the skull bone. Less invasive techniques can be done by threading a catheter. A catheter is guided through a small cut in the groin to an artery and then to the small blood vessels in the brain where the aneurysm is located. Thin metal wires are put into the aneurysm. They then coil up into a mesh ball. Blood clots that form around this coil prevent the aneurysm from breaking open and bleeding. If the aneurysm has ruptured, a clip may be placed on it to prevent further leaking of blood into the brain.
Managing Stroke Complications
In the days following stroke, patients are at risk for complications. The below steps are important.
Maintain Adequate Delivery of Oxygen. It is very important to maintain oxygen levels. In some cases, airway ventilation may be required. Supplemental oxygen may also be necessary for patients when tests suggest low blood levels of oxygen.
Manage Fever. Fever should be monitored and aggressively treated with medication and, if needed, a cooling blanket since its presence predicts a poorer outlook.
Evaluate Swallowing. Patients should have their swallowing function evaluated before they are given any food, fluid, or medication by mouth. If patients cannot adequately swallow they are at risk of choking. Patients who cannot swallow on their own may require nutrition and fluids delivered intravenously or through a tube placed in the nose.
Maintain Electrolytes. Maintaining a healthy electrolyte balance (the ratio of sodium, calcium, and potassium in the body's fluids) is critical.
Control Blood Pressure. Managing blood pressure is essential but complicated. Blood pressure often declines spontaneously in the first 24 hours after stroke. Patients whose blood pressure remains elevated should be treated carefully with antihypertensive medications.
Monitor Increased Brain Pressure. Hospital staff should watch closely for evidence of increased pressure on the brain (cerebral edema), which is a frequent complication of hemorrhagic strokes. It can also occur a few days after ischemic strokes. Early symptoms of increased brain pressure are drowsiness, confusion, lethargy, weakness, and headache. Medications such as mannitol may be given during a stroke to reduce pressure or the risk for it.
Keeping the top of the body higher than the lower part, such as by elevating the head of the bed, can reduce pressure in the brain and is standard practice for patients with ischemic stroke. However, this practice also lowers blood pressure in general, which may be dangerous for patients with massive stroke.
Monitor the Heart. Patients must be monitored using electrocardiographic tracings to check for atrial fibrillation and other heart rhythm problems. Patients are at high risk for heart attack following stroke.
Control Blood Sugar (Glucose) Levels. Elevated blood sugar (glucose) levels can occur with severe stroke and may be a marker of serious trouble. Patients with high blood glucose levels may require insulin therapy.
Monitor Blood Coagulation. Regular tests for blood coagulation are important to make sure that the blood is not so "thick" that it will clot nor so "thin" that it causes bleeding.
Check for Deep Venous Thrombosis. Deep venous thrombosis is a blood clot in the veins of the lower leg or thigh. It can be a serious post-stroke complication because there is a risk of the clot breaking off and traveling to the brain or heart. Deep venous thrombosis can also cause pulmonary embolism if the blood clot travels to the lungs. If necessary, an anticoagulant drug such as heparin may be given, but this increases the risk of hemorrhage. Patients who have had a stroke are also at risk for pulmonary embolisms
Prevent Infection. Patients who have had a stroke are at increased risk for pneumonia, urinary tract infections, and other widespread infections.
Prevention
Patients who have had a first stroke or TIA are at high risk of having another stroke. Secondary prevention measures are essential to reduce this risk.
Lifestyle Changes
Quit Smoking. Smoking is a major risk factor for stroke. Patients should also avoid exposure to second-hand smoke.
Eat Healthy. Patients should make dietary changes to follow a diet rich in fruits and vegetables, high in potassium, and low in saturated fats. Everyone should limit sodium (salt) intake to less than 1,500 mg/day. This is particularly important for people over age 50, all African-Americans, and everyone with high blood pressure. For diet plans, the Dietary Approaches to Stop Hypertension (DASH) diet, and the Mediterranean diet, may be particularly good choices for reducing the risk of stroke.
Exercise. Exercise helps reduce the risk of atherosclerosis, which can help reduce the risk of stroke. Doctors recommend at least 30 minutes of exercise on most, if not all, days of the week.
Maintain Healthy Weight. Patients who are overweight should try to lose weight through healthy diet and regular exercise.
Limit Alcohol Consumption. Heavy alcohol use and binge drinking increase the risk of both ischemic and hemorrhagic stroke. If you drink, limit alcohol to no more than one drink a day for women or two drinks a day for men.
Antiplatelet Medications for Preventing Stroke
Your doctor may suggest your taking aspirin or, if you cannot take aspirin, another antiplatelet drug such as clopidogrel (Plavix, generic) to help prevent blood clots from forming in your arteries or your heart. These medicines are called antiplatelet drugs. These drugs make blood platelets less sticky and therefore less likely to form a clot. You should never start taking aspirin without first talking to your doctor.
Primary Prevention (to prevent a first stroke). Primary prevention is when antiplatelet drugs are taken before a stroke or a TIA has occurred. Before deciding whether someone should take aspirin to prevent a stroke caused by a blockage in an artery (ischemic stroke), your doctor must consider whether you are at an increased risk of strokes caused by bleeding in the brain (hemorrhagic stroke), as well as bleeding elsewhere in the body.
- For men and women of any age who are considered at low risk for having a stroke, there is no evidence that taking aspirin will help prevent one.
- Women ages 55 - 79 years should consider taking low-dose aspirin (81 mg a day) if they are at risk for stroke or heart attack. Risk factors include high blood pressure, diabetes, smoking, a history of cardiovascular disease, atrial fibrillation, and left ventricular hypertrophy.
- Women who are younger than age 55 should not take aspirin simply for primary prevention of stroke.
- Men ages 45 - 79 years should consider taking aspirin if they are increased risk for heart attack. Aspirin is not recommended in men simply to prevent stroke. Some of the risk factors for coronary artery disease and heart attack are high blood pressure, diabetes, smoking, a history of cardiovascular disease, atrial fibrillation, and left ventricular hypertrophy.
- Men younger than age 45 should not take aspirin for primary prevention.
- For women and men age 80 years or older, it is not clear if the benefits of aspirin for stroke prevention outweigh the risks for bleeding in the digestive tract or brain.
- Daily use of aspirin can cause ulcers and gastrointestinal bleeding. Talk to your doctor about these risks.
Secondary Prevention (to prevent another stroke after one has occurred). After an ischemic stroke or a TIA, aspirin alone or aspirin plus the antiplatelet drug dipyridamole (Persantine, or Aggrenox when combined in one pill with aspirin) given twice daily is recommended to prevent another stroke. Clopidogrel may be used in place of aspirin for patients who have narrowing of the coronary arteries or who have had a stent inserted. Combining aspirin and clopidogrel together does not have any more benefit and increases the risk for hemorrhage.
Anticoagulant Medications for Preventing Stroke
Anticoagulants are also referred to as anti-clotting or “blood thinner” drugs. They are used to help prevent blood clots and stroke. They are generally considered the best medications for stroke prevention for most patients with atrial fibrillation who are at medium to high risk for stroke.
Warfarin. Warfarin (Coumadin, generic) has been the main anticoagulant (“blood thinner”) drug used to prevent strokes in high-risk patients with atrial fibrillation. Like all anticoagulants, warfarin carries a risk for bleeding, but for most patients its benefits far outweigh its risks. The risk for bleeding is highest when warfarin therapy is first started, with higher doses, and with long periods of treatment. Patients at risk for bleeding are usually older and have a history of stomach bleeding and high blood pressure.
It is important that patients who take warfarin have their blood checked regularly to make sure that it does not become “too thin.” Blood that is too thin increases the risk for bleeding, while blood that is “too thick” increases the risk for blood clots and stroke. Prothrombin time (PT) and international normalized ratio (INR) tests are used to monitor blood coagulation.
Patients who take warfarin need to be careful about the amount of vitamin K they consume from foods in their diet. Too much vitamin K can weaken warfarin’s effectiveness. Foods and beverages that are rich in vitamin K include kale, spinach, collard greens, mustard greens, chard, parsley, and green tea. Also, cranberry juice and alcohol can increase the effects of warfarin and the risks for bleeding. Talk with your doctor about any changes to your diet that you may need to make.
People with atrial fibrillation who are generally considered candidates for warfarin therapy often have one or more of the following characteristics:
- History of blood clots to the lungs, stroke, or transient ischemic attack
- Have a blood clot in one of their heart chambers
- Significant valvular heart disease
- High blood pressure
- Diabetes, with age older than 65 years
- Left atrium (one of the chambers of the heart) is enlarged
- Coronary artery disease
- Heart failure
- Age 75 years or older
Alternatives to Warfarin. In recent years, several new anticoagulants have been approved as alternatives to warfarin for preventing stroke and blood clots in patients with atrial fibrillation.
In 2010, the FDA approved dabigatran (Pradaxa) for patients with nonvalvular atrial fibrillation. According to recent guidelines from leading heart organizations, dabigatran is best suited for patients who do not have heart valve problems, kidney failure, or advanced liver disease.
Unlike warfarin, patients who take dabigatran do not need to have regular monitoring of their blood coagulation. However, dabigatran needs to be taken twice-daily (warfarin is taken once a day) and can cause a greater risk of certain types of side effects than warfarin. These non-bleeding side effects range from upset stomach to heart attack. Dabigatran is also more expensive than warfarin. Doctors currently recommend that patients who are doing well on warfarin may not benefit from switching to dabigatran. There have been reports that dabigatran may increase the risk of bleeding, but at the present time the FDA considers its benefits to outweigh its risks.
In 2011, the FDA approved Rivaroxaban (Xarelto) for stroke prevention in patients with nonvalvular atrial fibrillation. The FDA is expected to make a decision on a third new anticoagulant, apixaban (Eliquis), sometime in 2012.
Control Diabetes
People with diabetes should aim for fasting blood glucose levels of less than 110 mg/dl and hemoglobin A1C of around 7%. Blood pressure goals for people with diabetes should be 130/80 mm Hg or less.
Control Blood Pressure
Reducing blood pressure is essential in stroke prevention. Otherwise healthy patients with high blood pressure should aim for blood pressure below 140/90 mm Hg. Patients with diabetes, chronic kidney disease, or atherosclerosis should aim for blood pressure below 130/80 mm Hg. (However, these guidelines are being reevaluated.) Drug therapy is recommended for people with hypertension who cannot control their blood pressure through diet and other lifestyle changes. Many different types of drugs are used to control blood pressure. They include diuretics, ACE inhibitors, angiotensin-receptor blockers, beta-blockers, and calcium channel blockers.

Lower LDL Cholesterol
The American Heart Association recommends that patients who have had an ischemic stroke or TIA should take a statin drug to lower cholesterol levels. Most patients should aim to lower their LDL (“bad” cholesterol) to less than 100 mg/dL. Patients with multiple risk factors should aim for an LDL level of below 70 mg/dL.
Statin brands include lovastatin (Mevacor, generic), pravastatin (Pravachol, generic), simvastatin (Zocor, generic), fluvastatin (Lescol), atorvastatin (Lipitor, generic), rosuvastatin (Crestor), and pitavastatin (Livalo).
Surgery
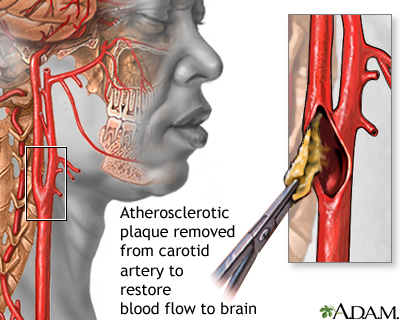
Carotid Endarterectomy
Carotid endarterectomy is a surgical procedure that cleans out plaque and opens up the narrowed carotid arteries in the neck. It is recommended to prevent ischemic stroke in some patients who have symptoms of carotid artery stenosis and carotid narrowing of 70% or more. For people whose carotid arteries are narrowed by 50% or less, antiplatelet medications are usually recommended in place of surgery. For patients with moderate stenosis (50 - 69%), the decision to perform surgery needs to be determined on an individual basis.
There is a risk of a heart attack or stroke from the procedure. Anyone undergoing this procedure should be sure their surgeon is experienced in performing this procedure and that the medical center has complication rates of less than 6%. Carotid endarterectomy is generally not recommended for patients with acute stroke.
Procedure Description. A carotid endarterectomy involves:
- The patient is usually given general anesthesia, although a local anesthetic is sometimes used.
- The surgeon cuts open the carotid artery and scrapes away the plaque on the arterial wall.
- The artery is sewn back together, and blood flow is restored.
- The patient generally stays in the hospital for about 1 - 2 days.
- There is often a slight aching in the neck for about 2 weeks, and the patient should refrain as much as possible from turning the head during this period. Patients may temporarily lose sensation in the neck area. It will go away within a few months.
Carotid Angioplasty and Stenting
Carotid angioplasty and stenting (CAS) may be used as an alternative to carotid endarterectomy for some patients. It is based on the same principles as angiography done for heart disease.
- An extremely thin catheter tube is inserted into an artery in the groin.
- It is threaded through the circulatory system until it reaches the blocked area in the carotid artery.
- The doctor either breaks up the clot or inflates a tiny balloon against the blood vessel walls (angioplasty).
- After temporarily inflating the balloon, the doctor typically leaves a circular wire mesh (stent) inside the vessel to keep it open.
This procedure carries a risk for an embolic stroke and other complications. At this time, it is mainly used in some hospitals as an alternative procedure for patients who cannot undergo endarterectomy, especially for patients with severe stenosis (blockage greater than 70%) and high surgical risk. Some recent research has indicated that extracranial carotid stenting may work as well as carotid endarterectomy in high-risk patients younger than age 70. However, other studies have found that stenting increases the risk of adverse effects.
Carotid artery stenting involves placement of the stent in the neck as a treatment for extracranial (outside the skull) carotid artery stenosis. Another type of stenting procedure, percutaneous transluminal angioplasty and stenting (PTAS), has been investigated as a treatment for preventing stroke in patients with intracranial (inside the skull) arterial stenosis. The PTAS procedure is similar to CAS, but it involves positioning a stent to prop open blocked arteries within the brain, not the carotid artery in the neck.
In 2011, an important trial found that patients treated with PTAS experienced many more strokes than patients who carefully controlled risk factors (like high blood pressure and cholesterol) and took antiplatelet medications like aspirin and clopidogrel. Another type of surgical treatment for stroke prevention – the extracranial-intracranial bypass – also does not appear effective for stroke prevention in patients with a completely blocked carotid artery. The results of these trials suggest that for most patients, medical treatment with drug therapy is the best way to prevent recurrent strokes.
Rehabilitation
Most people who survive a stroke will have some type of disability. But many people are able to make significant improvements through rehabilitation. According to the National Stroke Association:
- 10% of stroke survivors recover almost completely
- 25% recover with minor impairments
- 40% experience moderate-to-severe impairments that require special care
- 10% require care in a nursing home or other long-term facility
For the best chance of improvement and regaining abilities, it is important that rehabilitation starts as soon as possible after a stroke. Rehabilitation therapy is started in the hospital as soon as a patient’s condition has stabilized. Initial range of motion exercises involve a nurse or physical therapist moving a patient’s affected limb (passive exercise) and having the patient practice moving the limb (active exercise). Patients are encouraged to gradually sit, stand, and walk, and then perform tasks of daily living (such as bathing, dressing, and using the toilet).
Some patients will experience recover quickly and regain functional abilities in the first few days, while others will continue to show improvement during the first 6 months or longer. Recovery is an ongoing process and with good rehabilitation providers and family support, patients can continue to make progress.
Rehabilitation Services
Once a patient has been discharged from the hospital, rehabilitation continues at home or in an outpatient program. Some patients may be transferred to a rehabilitation hospital before going home. Others may require care in a long-term or skilled nursing facility. In addition to the ongoing care of a primary care physician or neurologist, a rehabilitation team may include:
- Physical therapists who focus on restoring physical function and helping patients improve strength, balance, and coordination
- Occupational therapists to help patients regain ability to perform activities of daily living
- Speech-language therapists to help improve language skills
- Psychologists to help with the patient’s mental and emotional state
- Social workers to help patients and families with financial arrangements and coordinating home services
Effects of Stroke
A stroke can cause various disabilities. The type of disability depends on which part of the brain was damaged. According to the U.S. National Institutes of Health, the five main types of stroke disabilities are:
- Paralysis or Problems Controlling Movement (Motor Control). Paralysis tends to occur on opposite side of the body from the side of the brain damage. If someone has brain damage on the left side of the brain, the right side of the body will be affected, and the reverse is also true. One-sided paralysis is called hemiplegia, and one-sided weakness is called hemiparesis. Hemiplegia or hemiparesis can affect a person’s ability to walk or grasp objects. Loss of muscle control can also cause problems swallowing (dysphagia) or speaking (dysarthria). Patients may also have difficulty with coordination and balance (ataxia).
- Sensory Disturbances Including Pain. Stroke can affect the ability to feel touch, pain, temperature, or position. Pain, numbness, and tingling or pricking sensations can occur in the paralyzed or weakened limb (paresthesia). Sometimes patients have problems recognizing their affected arm or leg. Some stroke survivors experience chronic pain, which often results from a joint becoming immobilized or “frozen." Muscle stiffness or spasms are common. Sensory disturbances can also affect the ability to urinate or control bowels.
- Problems Using or Understanding Language (Aphasia). Many stroke survivors have language impairments, which affect the ability to speak, write, and understand spoken or written language. This condition is called aphasia. Sometimes patients will know the right words but have problems saying them (dysarthria).
- Problems with Thinking and Memory. Stroke can affect attention span and short-term memory. This can impair the ability to make plans, learn new tasks, follow instructions, or comprehend meaning. Some stroke survivors are unable to recognize or understand their physical impairments or are unaware of sensations affecting the stroke-impaired side of the body.
- Emotional Disturbances. Some emotional and personality changes that follow a stroke are caused by the effects of brain damage. Clinical depression is very common, and is not only a psychological response to stroke but a symptom of physical changes in the brain. Patients may have difficulty controlling emotions or may exhibit inappropriate emotional responses (crying, laughing, or smiling for no apparent reason).
Rehabilitation Programs
Because stroke affects different parts of the brain, specific approaches to managing rehabilitation vary widely among individual patients:
- Exercise program. Guidelines from the Veteran’s Administration recommend that patients get back on their feet as soon as possible to prevent deep vein thrombosis. Patients should try to walk at least 50 feet a day. Assisted devices or bracing are sometimes used to help support the legs. Treadmill exercises can be very helpful for patients with mild-to-moderate dysfunction. Exercise should be tailored to the stroke survivor's physical condition and can include aerobic, strength, flexibility, and neuromuscular (coordination and balance) activities.
- Retraining muscles. Stretching and range-of-motion exercises are used to help treat spastic muscles. They can also help patients regain function in a paralyzed arm. Multiple techniques have been developed and studied.
- Speech therapy and sign language. Intense speech therapy after a stroke is important for recovery. Some doctors recommend 9 hours a week of therapy for 3 months. Language skills improve the most when family and friends help reinforce the speech therapy lessons.
- Swallowing training. Training patients and their caregivers regarding swallowing techniques, as well as safe and not-safe foods and liquids, is essential for preventing aspiration (accidental sucking in of food or fluids into the airway).
- Attention training. Problems with attention are very common after strokes. Direct retraining teaches patients to perform specific tasks using repetitive drills in response to certain stimuli. (For example, they are told to press a buzzer each time they hear a specific number.) A variant of this approach trains patients to relearn real-life skills, such as driving, carrying on a conversation, or other daily tasks.
- Occupational training. Occupational therapy is important and improves daily living activities and social participation.
Drug Therapy for Rehabilitation
Medication can sometimes help relieve specific effects of stroke:
- Dantrolene (Dantrium, generic), tizanidine (Zanaflex, generic), and baclofen (Lioresel, Gablofen, generic) are used to treat spasticity. Botox injections are approved for treatment of upper limb spasticity (such as the elbow, wrist, or fingers).
- Heparin, a blood-thinning drug, is used to prevent blood clots from forming in the veins of the legs (thrombosis).
- Some patients experience constant hiccups, which can be very serious. Chlorpromazine and baclofen are among the drugs used for this condition.
- Antidepressants may be prescribed for treatment of depression.
Managing the Emotional Consequences
A stroke is emotionally challenging both for patients and their families. The caregiver's emotions and responses to the patient are critical. Patients do worse when caregivers are depressed, overprotective, or not knowledgeable about the stroke. They do best when caregivers and family are encouraging and supportive. Everyone benefits when patients are able to function as independently as possible to the best of their abilities.
Resources
- www.strokeassociation.org -- American Stroke Association
- www.heart.org -- American Heart Association
- www.stroke.org -- National Stroke Association
- www.ninds.nih.gov -- National Institute of Neurological Disorders and Stroke
- www.aphasia.org -- National Aphasia Association
- www.aan.com -- American Academy of Neurology
- www.strokecenter.org -- Internet Stroke Center
References
Adams HP Jr. Secondary prevention of atherothrombotic events after ischemic stroke. Mayo Clin Proc. 2009;84(1):43-51.
Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007 May 22;115(20):e478-534.
Amarenco P, Goldstein LB, Szarek M, Sillesen H, Rudolph AE, Callahan A 3rd, et al. Effects of intense low-density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke. 2007 Dec;38(12):3198-204. Epub 2007 Oct 25.
Bederson JB, Connolly ES Jr, Batjer HH, Dacey RG, Dion JE, Diringer MN, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 2009 Mar;40(3):994-1025. Epub 2009 Jan 22.
Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM, Brooks W, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010 Jul 1;363(1):11-23. Epub 2010 May 26.
Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011 Sep 15;365(11):993-1003. Epub 2011 Sep 7.
Del Zoppo GJ, Saver JL, Jauch EC, Adams HP Jr; American Heart Association Stroke Council. Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke. 2009 Aug;40(8):2945-8. Epub 2009 May 28.
Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009 Jun;40(6):2276-93. Epub 2009 May 7.
Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011 Jan;42(1):227-76. Epub 2010 Oct 21.
Goldstein LB. Prevention and management of stroke. In: Bonow RO, Mann DL, Zipes DP, Libby P, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Saunders; 2012:chap 62. .
Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011 Feb;42(2):517-84. Epub 2010 Dec 2.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011 Sep 15;365(11):981-92. Epub 2011 Aug 27.
Halliday A, Harrison M, Hayter E, Kong X, Mansfield A, Marro J, et al. 10-year stroke prevention after successful carotid endarterectomy for asymptomatic stenosis (ACST-1): a multicentre randomised trial. Lancet. 2010 Sep 25;376(9746):1074-84.
Lansberg MG, O'Donnell MJ, Khatri P, Lang ES, Nguyen-Huynh MN, Schwartz NE, et al. Antithrombotic and thrombolytic therapy for ischemic stroke: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e601S-36S.
Latchaw RE, Alberts MJ, Lev MH, Connors JJ, Harbaugh RE, Higashida RT, et al. Recommendations for imaging of acute ischemic stroke: a scientific statement from the American Heart Association. Stroke. 2009 Nov;40(11):3646-78. Epub 2009 Sep 24.
Legg L, Drummond A, Leonardi-Bee J, Gladman JR, Corr S, Donkervoort M, et al. Occupational therapy for patients with problems in personal activities of daily living after stroke: systematic review of randomised trials. BMJ. 2007 Nov 3;335(7626):922. Epub 2007 Sep 27.
Morgenstern LB, Hemphill JC 3rd, Anderson C, Becker K, Broderick JP, Connolly ES Jr, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010 Sep;41(9):2108-29. Epub 2010 Jul 22.
Myint PK, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Combined effect of health behaviours and risk of first ever stroke in 20,040 men and women over 11 years' follow-up in Norfolk cohort of European Prospective Investigation of Cancer (EPIC Norfolk): prospective population study. BMJ. 2009 Feb 19;338:b349. doi: 10.1136/bmj.b349.
O'Regan C, Wu P, Arora P, Perri D, Mills EJ. Statin therapy in stroke prevention: a meta-analysis involving 121,000 patients. Am J Med. 2008 Jan;121(1):24-33.
Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA. 2011 Sep 21;306(11):1241-9.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011 Sep 8;365(10):883-91. Epub 2011 Aug 10.
Powers WJ, Clarke WR, Grubb RL Jr, Videen TO, Adams HP Jr, Derdeyn CP; et al. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA. 2011 Nov 9;306(18):1983-92.
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012 Jan 3;125(1):e2-e220. Epub 2011 Dec 15.
Silver FL, Mackey A, Clark WM, Brooks W, Timaran CH, Chiu D, et al. Safety of stenting and endarterectomy by symptomatic status in the Carotid Revascularization Endarterectomy Versus Stenting Trial (CREST). Stroke. 2011 Mar;42(3):675-80. Epub 2011 Feb 9.
Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011 Nov 29;58(23):2432-46. Epub 2011 Nov 3.
Summers D, Leonard A, Wentworth D, Saver JL, Simpson J, Spilker JA, et al. Comprehensive overview of nursing and interdisciplinary care of the acute ischemic stroke patient: a scientific statement from the American Heart Association. Stroke. 2009 Aug;40(8):2911-44. Epub 2009 May 28.
US Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009 Mar 17;150(6):396-404.
Wann LS, Curtis AB, Ellenbogen KA, Estes NA 3rd, Ezekowitz MD, Jackman WM, et al. 2011 ACCF/AHA/HRS Focused Update on the Management of Patients With Atrial Fibrillation (Update on Dabigatran): A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011 Mar 15;123(10):1144-50. Epub 2011 Feb 14.
Wann LS, Curtis AB, January CT, Ellenbogen KA, Lowe JE, Estes NA 3rd, et al. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (updating the 2006 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011 Jan 4;123(1):104-23. Epub 2010 Dec 20.
Wolff T, Guirguis-Blake J, Miller T, Gillespie M, Harris R. Screening for carotid artery stenosis: an update of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2007 Dec 18;147(12):860-70.
You JJ, Singer DE, Howard PA, Lane DA, Eckman MH, Fang MC, et al. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e531S-75S.
|
Review Date:
5/28/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |







